|
Recent statistics suggest that sudden cardiac arrest is rapidly becoming the leading cause of death in America. Once the heart ceases to function, a healthy human brain may survive without oxygen for up to 4 minutes without suffering any permanent damage. Unfortunately, a typical EMS response may take 6, 8 or even 10 minutes.
It is during those critical minutes that Cardio Pulmonary Resuscitation can provide oxygenated blood to the victim's brain and the heart, dramatically increasing his chance of survival. And if properly instructed, almost anyone can learn and perform CPR.
|
|
HOW CPR WORKS
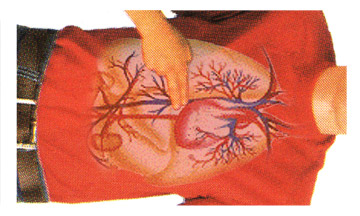
The air we breathe in travels to our lungs where oxygen is picked up by our blood and then pumped by the heart to our tissue and organs. When a person experiences cardiac arrest - whether due to heart failure in adults and the elderly or an injury such as near drowning, electrocution or severe trauma in a child - the heart goes from a normal beat to an arrhythmic pattern called ventricular fibrillation, and eventually ceases to beat altogether. This prevents oxygen from circulating throughout the body, rapidly killing cells and tissue. In essence, Cardio (heart) Pulmonary (lung) Resuscitation (revive, revitalize) serves as an artificial heartbeat and an artificial respirator.
CPR may not save the victim even when performed properly, but if started within 4 minutes of cardiac arrest and defibrillation is provided within 10 minutes, a person has a 40% chance of survival (figure 1).
|

figure 1
|
|
Invented in 1960, CPR is a simple but effective procedure that allows almost anyone to sustain life in the first critical minutes of cardiac arrest. CPR provides oxygenated blood to the brain and the heart long enough to keep vital organs alive until emergency equipment arrives. To make learning CPR easier, a system was devised that makes remembering it as simple as "ABC":
- Airway
- Breathing
- Circulation
WHEN TO DIAL 9-1-1
It is critical to remember that dialing 9-1-1 may be the most important step you can take to save a life. If someone besides you is present, they should dial 9-1-1 immediately. If you're alone with the victim, try to call for help prior to starting CPR on an adult and after a minute on a child. Before we learn what to do in an emergency, we must first emphasize what NOT to do:
- DO NOT leave the victim alone.
- DO NOT try to make the victim drink water.
- DO NOT throw water on the victim's face.
- DO NOT prompt the victim into a sitting position.
- DO NOT try to revive the victim by slapping his face.
Always remember to exercise solid common sense. When faced with an emergency situation we may act impulsively and place ourselves in harm's way. Although time should not be wasted, only approach the victim after determining that the scene is safe: always check for cars, fire, gas, downed electrical lines, and any other potential hazards before attempting to perform CPR.
|
ADULT CPR
Definition
American Heart Association's guidelines dictate that Adult CPR is performed on any person over the age of 8. The procedure outlined in the following lessons is similar to Children CPR and Infant CPR, although some critical differences apply. Before you start any rescue efforts, you must remember to check the victim for responsiveness.
Assessing the situation
If you suspect that the victim has sustained spinal or neck injury, do not move or shake him. Otherwise, shake the victim gently and shout "Are you okay?" to see if there is any response. If the victim is someone you know, call out his name as you shake him. If there is no response, immediately dial 9-1-1 and check the airway.
|
|
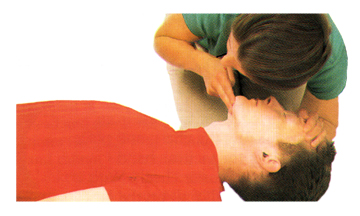
A-B-C of Adult CPR
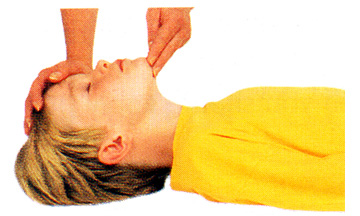
"A" is for AIRWAY. If the victim is unconscious and is unresponsive, you need to make sure that his airway is clear of any obstructions. The breaths may be faint and shallow - look, listen and feel for any signs of breathing (figure 1). If you determine that the victim is not breathing, then something may be blocking his air passage. The tongue is the most common airway obstruction in an unconscious person and it may be necessary to perform a finger sweep in order to move the tongue or any other foreign object away from the air passage. With the victim lying flat on his back, firmly hold his chin with one hand while using the finger of your other hand in a sweeping motion (figure 2).
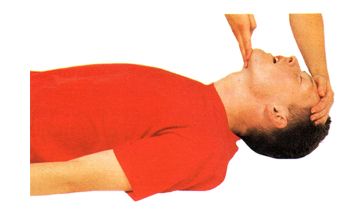
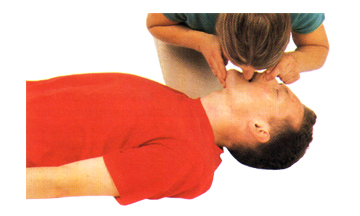
Once the airway is unblocked, place your hand on victim's forehead and your other hand under the tip of the chin and gently tilt his head backward (figure 3). In this position the weight of the tongue will force it to shift away from the back of the throat, opening the airway. If the person is still not breathing on his own after the airway has been cleared, you will have to assist him breathing.
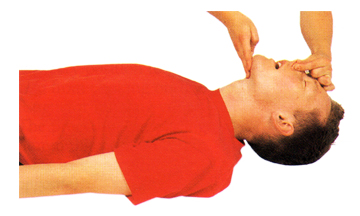
"B" is for BREATHING. With the victim's airway clear of any obstructions, gently support his chin so as to keep it lifted up and the head tilted back. Pinch his nose to prevent air from escaping once you begin to ventilate (figure 4). Take a full breath, place your mouth tightly over the victim's (use a shield barrier if one is available) and blow (figure 5) until the victim's chest rises. Maintain a tight seal around his mouth and be careful not to over-inflate his lungs as this may force air into the stomach, causing him to vomit. If this happens, turn the victim's head to the side and sweep any obstructions out of the mouth before proceeding.
Between each breath allow the victim's lungs to relax - place your ear near his mouth and listen for air to escape and watch the chest fall as he exhales. If the victim remains unresponsive (no breathing, coughing or moving), check his circulation.
"C" is for CIRCULATION. In order to determine if the victim's heart is beating, place two fingertips on his carotid artery, located in the depression between the windpipe and the neck muscles, and apply slight pressure for several seconds. If there is no pulse then the victim's heart is not beating, and you will have to perform chest compressions.
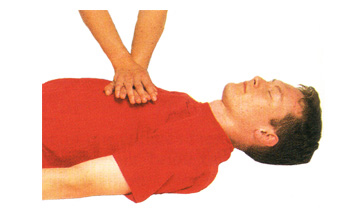
Chest compressions
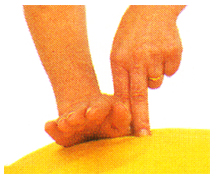
When performing chest compressions, proper hand placement is very important. Place two fingers on the victim's sternum (figure 6) and then put the heel of your other hand next to your fingers (figure 7). Now you need to place your hand on top of that hand and interlace the fingers (figure 8).
|
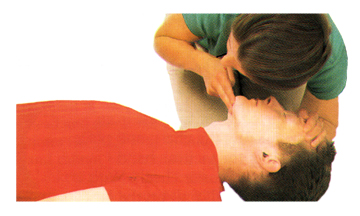
figure 1

figure 2
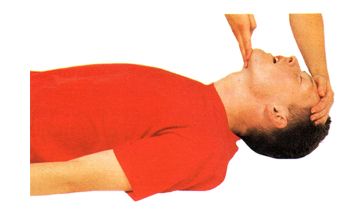
figure 3
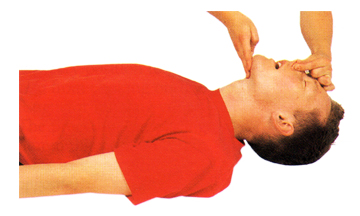
figure 4
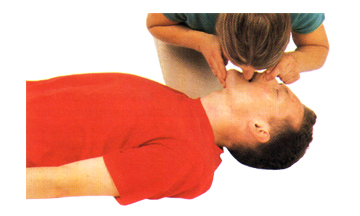
figure 5
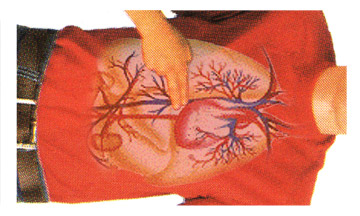
figure 6

figure 7
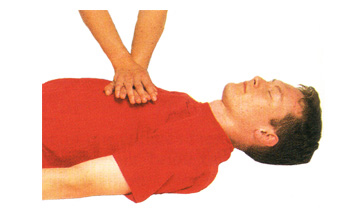
figure 8
|
|
Lock your elbows and using your body's weight, compress the victim’s chest. The depth of compressions should be approximately 1½ to 2 inches - remember: 2 hands, 2 inches. If you feel or hear slight cracking sound, you may be pressing too hard. Do not become alarmed and do not stop your rescue efforts! Damaged cartilage or cracked ribs are far less serious then a lost life. Simply apply less pressure as you continue compressions.
Count aloud as you compress 15 times at the rate of about 3 compressions for every 2 seconds. Finish the cycle by giving the victim 2 breaths. This process should be performed four times - 30 compressions and 2 breaths - after which remember to check the victim's carotid artery for pulse and any signs of consciousness.
What to do next
If there is no pulse, continue performing 30 compressions/2 breaths, checking for pulse after every 4 cycles until help arrives. If you feel a pulse (i.e. the victim's heart is beating) but the victim is still not breathing, rescue breaths should be administered, one rescue breath every five seconds (remember to pinch the nose to prevent air from escaping). After the first rescue breath, count five seconds and if the victim does not take a breath on his own, give another rescue breath.
|
CHILD CPR
Definition
According to American Heart Association's guidelines Child CPR should be administered to any victim under the age of 8. Although some of the material in the next lesson may seem repetitive, we strongly recommend that you do not skip ahead as there are crucial distinctions that apply to rescue efforts for children.
Assessing the situation
The first thing to remember about Child CPR is this: in children cardiac arrest is rarely caused by heart failure but rather by an injury such as poisoning, smoke inhalation, or head trauma, which causes the breathing to stop first. And since children are more resilient than adults statistics have shown that they tend to respond to CPR much better if administered as soon as possible. If the child is unresponsive and you are alone with him, start rescue efforts immediately and perform CPR for at least 1 to 2 minutes before dialing 9-1-1.
Before you call an ambulance, immediately check the victim for responsiveness by gently shaking the child and shouting, "Are you okay?" DO NOT shake the child if you suspect he may have suffered a spinal injury. If the child is clearly unconscious, remember your A-B-C and check the child's airway.
|
A-B-C of Child CPR
"A" is for AIRWAY. A child's breaths may be extremely faint and shallow - look, listen and feel for any signs of breathing. If there are none, the tongue may be obstructing the airway and preventing the child from breathing on his own. Exercise extra caution when you open the victim's air passage using the head tilt/chin lift technique (figure 1). This will shift the tongue away from the airway. If the child is still not breathing after his airway has been cleared, you will have to assist him in breathing.
"B" is for BREATHING. If the child remains unresponsive and still not breathing on his own, pinch his nose with your fingertips or cover his mouth and nose with your mouth creating a tight seal, and give two breaths (figure 2).
Keep in mind that children's lungs have much smaller capacity than those of adults. When ventilating a child, be sure to use shallower breaths and keep an eye on the victim's chest to prevent stomach distention. If this happens and the child vomits, turn his head sideways and sweep all obstructions out of the mouth before proceeding.
"C" is for CIRCULATION. Check the child's carotid artery for pulse by placing two fingertips and applying slight pressure on his carotid artery for approximately 5 to 10 seconds. If don't feel a pulse then the victim's heart is not beating, and you will have to perform chest compressions.
Chest compressions
When performing chest compressions on a child proper hand placement is even more crucial than with adults. Place two fingers at the sternum and then put the heel of your other hand directly above your fingers (figure 3). A child's smaller and more fragile body requires less pressure when performing compressions. The rule to remember is 1 hand, 1 inch (figure 4).
|
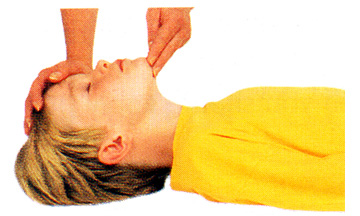
figure 1

figure 2
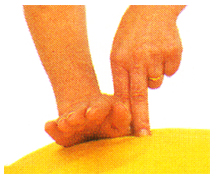
figure 3

figure 4
|
If you feel or hear slight cracking sound, you may be pressing too hard. Apply less pressure as you continue. Count aloud as you compress five times, followed by one breath. Perform this cycle 20 times - five chest compressions followed by one breath - after which remember to check the victim's carotid artery for pulse as well as any signs of consciousness.
What to do next
NOW IS THE TIME TO DIAL 9-1-1. Return to the child as quickly as possible. If there is still no pulse, repeat a complete cycle of 30 compressions/2 breaths 20 times before checking for pulse and breathing. If none are present, continue performing CPR until help arrives. If the child regains an active heartbeat (you detect a pulse) but is still not breathing, rescue breaths at the rate of 1 breath every 3 seconds need to be administered (remember to pinch the nose to prevent air from escaping). After the first rescue breath, count three seconds and if the child does not take a breath on his own, give another rescue breath.
|
INFANT CPR
Definition
According to generally accepted guidelines, Infant CPR is administered to any victim under the age of 12 months. Infants, just as children, have a much better chance of survival if CPR is performed immediately. If you are alone with the infant, do not dial 9-1-1 until after you have made an attempt to resuscitate the victim.
Assessing the situation
Check the infant for responsiveness by patting his feet and gently tapping his chest or shoulders. If he does not react (stirring, crying, etc.), immediately check his airway.
|
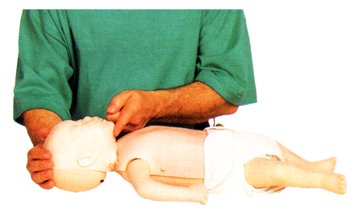
A-B-C of Infant CPR
"A" is for AIRWAY. It is normal for an infant to take shallow and rapid breaths, so carefully look, listen and feel for breathing. If you cannot detect any signs of breathing, the tongue may be obstructing the infant's airway.
Although the head tilt/chin lift technique is similar to adults and children, when clearing an infant's airway it's important not to tilt the head too far back. An infant's airway is extremely narrow and overextending the neck may actually close off the air passage (figure 1).
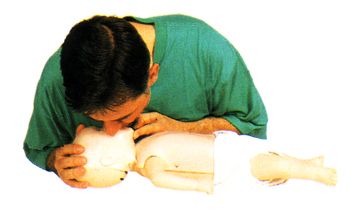
"B" is for BREATHING. To artificially respirate an infant, place your mouth over his mouth and nose and give a gentle puff from your cheeks (figure 2). Let the victim exhale - watch his chest and listen and feel for breathing. If he does not breathe on his own, again place your mouth over his mouth and nose and give another small puff. If the infant remains unresponsive (no crying or moving), immediately check his circulation.
"C" is for CIRCULATION. An infant's pulse is checked at the brachial artery which is located inside of the upper arm, between the elbow and the shoulder.
Locate the artery and place two fingers on it, applying slight pressure for 3 to 5 seconds. If you do not feel a pulse within that time, then the infant's heart is not beating, and you will need to perform chest compressions.
|
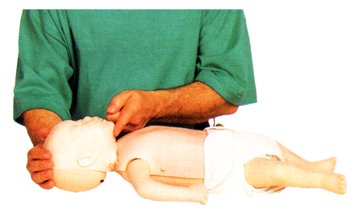
figure 1
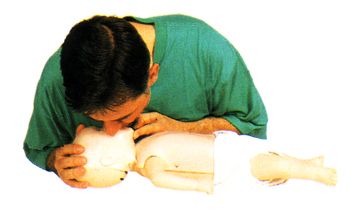
figure 2
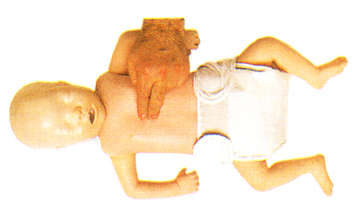
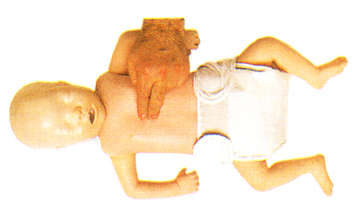
figure 3
|
Chest compressions
An infant's delicate ribcage is especially susceptible to damage if chest compressions are improperly performed, therefore it is important to use caution when rescuing an infant. With the infant flat on his back, place two fingers in the center of his chest at the level of the nipples (figure 3). The compression should be approximately ½ inch deep - remember, ½ hand (2 fingers), ½ inch. Count aloud as you perform five compressions and follow up with one breath. Repeat this cycle 20 times before checking the infant for breathing and pulse.
What to do next
NOW IS THE TIME TO DIAL 9-1-1. Return to the victim as promptly as possible. If he still has no pulse, continue administering 5 compressions/1 breath until EMS arrives. If at any point the infant regains a pulse but still does not breathe on his own, give him one rescue breath every 3 seconds.
|
|
BASIC FIRT AID
We all take certain measures to prevent accidents but despite our best efforts emergencies arise. You trip and fall... unintentionally come in contact with exposed wiring... step on a rusty nail... or literarily bite off more than you can chew... And when an accident happens, time is not on your side. Besides a well-stocked and functional First Aid Kit, preparation and skills are the most important tools you can have at your disposal.
This section of our on-line course will introduce you to a number of common emergency situations and their respective First Aid responses. Feel free to return to any area of this section as many times as you feel are necessary until you feel comfortable that should an accident happen, you are well equipped to deal with it appropriately.
A good First Aid Kit (figure 1) should be checked and restocked periodically and should always contain the following items:
|
- Sterile adhesive bandages in assorted sizes
- Sterile gauze pads in assorted sizes
- Hypoallergenic adhesive tape
- Scissors
- Tweezers
- Needle
- Ace bandage
- Moistened towelettes
- Antiseptic
- Thermometer
- Tongue blades
- Splints in assorted sizes
- Petroleum jelly
- Assorted sizes of safety pins
- Anti-bacterial soap
- Antibiotic ointment
- Latex gloves and face mask
- Sunscreen
- Aspirin and/or ibuprofen
- Ice Pack
|

figure 1
|
BASIC FIRST AID: BITE WOUNDS
If the victim was bitten by an unprovoked undomesticated animal such as a raccoon or a squirrel, an immediate shot may be necessary to prevent the possibility of a rabies infection.
Contrary to common belief, a human bite can sometimes be more dangerous than that of an animal because human saliva contains many more types of bacteria which may cause infection.
A bite from a domestic pet can be painful but rarely requires a visit to the emergency room and unless obvious bodily harm was sustained, a simple precautionary treatment will suffice.
- Use anti-bacterial soap and water to thoroughly clean the bite wound.
- Apply antibiotic ointment such as Neosporin to prevent infection.
- If the injury resulted in broken skin, dress it with a sterile bandage and
- replace the dressing frequently.
- If the bite is deep, the victim may need to be treated for a puncture wound.
|
BASIC FIRST AID: BROKEN BONE
A broken bone may not always be obvious as most breaks do not result in compound fractures (bone protruding through the skin). It is important not to misdiagnose a break and mistake it for a bruise or sprain. Typical symptoms of a broken bone are:
- Immediate and excessive swelling
- Injured area appears deformed
- The farthest point of the injured limb turns blue or is numb to the touch
- Even slight movement or contact to the injured area causes excessive pain
Dial 9-1-1 immediately and immobilize the broken bone with a splint. A functional splint can be made of almost any material (wood, plastic, etc.) as long as it is rigid and is longer than the broken bone. To apply the splint simply lay it along the broken bone and wrap it against the limb with gauze or a length of cloth, starting at a point farthest from the body. Do not wrap it too tight as this may cut off blood flow.
If the break is in the forearm, loosely wrap a magazine or a thick newspaper around the break and use a sling fashioned from gauze or a strip of cloth to keep the elbow immobilized.
A break in the lower part of the leg requires two splints, one on each side of the leg (or at least the chin). If suitable material is not available, you can use the victim's healthy leg as a makeshift splint.
As much as possible, keep the victim from moving and until an ambulance arrives, remember ICE:
- "I" is for ice - if possible apply an ice pack or ice cubes to the injured area. This will keep down the swelling and reduce pain.
- "C" is for compression - if the wound is bleeding, apply direct pressure with a clean cloth to reduce blood flow.
- "E" is for elevation - try to keep the injured area as high above heart level as possible. This will reduce blood flow to the injury and minimize swelling.
|
BASIC FIRST AID: BRUISE
A typical bruise is a contusion caused by traces of blood escaping from small vessels that lie close to the skin's surface. Since our blood vessels become more fragile with age, the elderly tend to bruise easier than healthy adults and children. Conversely, if a child sustains excessive bruising, it may be an indication of a more serious injury and should be treated accordingly.
If the bruise is on the victim's head and noticeable swelling occurs, he should be checked for head trauma.
To reduce the bump and minimize the pain, have the victim elevate the injured area and apply a commercial ice pack or ice cubes wrapped in a towel for 30 to 45 minutes. Depending on the extent of the injury, this process should be repeated for a few days or until the swelling and the pain begin to dissipate.
|
BASIC FIRST AID: BURN
A burn victim will require different type of care depending on the type and extent of his injury. Burns vary greatly from a common, fairly harmless sunburn to a potentially life-threatening 3rd degree burn caused by open flames or electrocution [show me]. Here's how to distinguish the three different types of burn injuries and how to care for each:
- 1st degree burns are usually accompanied by redness and some swelling of the skin. Treat a minor burn by first cooling the affected area. If possible, keep the injury under cool running water for at least 10 minutes. If running water is not available place the burn in a container of cold water such as a bucket, tub or even a deep dish. Using a cool, wet compress made of clean cloth will also work if nothing else is available. Keeping the burn cool will reduce pain and minimize the swelling. If the injury is on the part of a body where jewelry or snug clothing is present, carefully remove them before it begins to swell. Apply a moisturizing lotion or Aloe Vera extract and dress the burnt area with loosely wrapped sterile gauze.
- 2nd degree burns will result in deeper, more intense redness of the skin as well as swelling and blistering. This type of burn should be treated just as a 1st degree burn but because the damage to the skin is more extensive, extra care should be taken to avoid infection and excessive scarring. Replace the dressing daily and keep the wound clean. If a blister breaks use mild soap and warm water to rinse the area. Apply antibiotic cream such as Neosporin to prevent infection before redressing in sterile gauze.
- 3rd degree burns may appear and feel deceptively harmless as the victim may not feel much pain due to complete destruction of all layers of skin and tissue as well as nerve endings. The damaged area may appear charred or ash-color and will instantly start to blister or "peel". If the victim's clothing is on fire, douse him with non-flammable liquid. Dial 9-1-1. Do not remove burnt clothing from the victim as this will expose open wounds to the elements and potential infection. If possible, cover the victim's injuries with wet sterile cloth to reduce the pain and swelling. If you notice that the victim is going into shock and loses consciousness, you will need to perform CPR.
|
BASIC FIRST AID: CHOKING
Choking is usually caused by a piece of foreign matter such as food becoming lodged in a person's windpipe. Because a choking victim is fully aware that he cannot breathe normally, a sense of panic may overcome them, making assessing the situation and rescue efforts difficult. It is important to try and keep the victim calm in order to determine whether your assistance is truly necessary or if the victim's own coughing reflex is sufficient.
Start by asking the person if he is choking. This simple step can be deceptively effective - the victim may be coughing violently or even gasping for air, but if he is able to answer then he is probably not choking. A choking victim will not be able to speak since oxygen cannot reach his lungs. But if after asking the person if he's choking all he can do is gesture or point to his throat and you notice his face starting to turn blue, then he is most likely choking and you will need to perform the Heimlich Maneuver immediately.
- Start by finding the proper stance - behind the victim with one of your feet planted firmly between the victim's feet.
- Wrap one of your arms around the victim and place your hand in a closed fist just slightly above his belly button.
- Place your other hand directly on top of the first.
- Squeeze the victim's abdomen in quick upward thrusts as many times as it is necessary to dislodge the object in his windpipe.
|
BASIC FIRST AID: CUTS
The first and possibly most important step when treating minor cuts and scrapes is to thoroughly clean the wound with mild anti-bacterial soap and water. You can use sterilized tweezers to remove any debris that remains embedded in the wound after rinsing. This will reduce the risk of an infection and possible complications. If the debris is abundant or can't be removed for some other reason, a trip to the emergency room will be necessary.
Water may induce bleeding by thinning the blood. If while rinsing the wound you notice increased blood flow, use gauze or a clean cloth to apply gentle, continuous pressure until the blood clots.
Although hydrogen peroxide is commonly used as a disinfectant for minor cuts and scrapes, it is actually not very effective and may even delay the healing process by irritating a person's living cells. You can use hydrogen peroxide but apply it around the open wound, not directly to it. An antibiotic ointment such as Neosporin is a better alternative - it will keep the wound from getting infected and speed up the healing process.
Dress the wound with a bandage or sterile gauze to keep dirt and bacteria out. Change the dressing frequently and rinse the wound as often as necessary to keep it free of dirt.
Continue to monitor the wound for several days. If the injured area turns red or puffy, or if excessive pain persists, then it may've become infected and will require a physician's attention. Do not simply dismiss cuts as minor injuries as some may be quite serious if not tended to by a professional. If the wound is very deep or the bleeding is profuse, it may require stitches in order to heal properly.
|
BASIC FIRST AID: ELECTROCUTION
Electricity travels through conductors - any material which allows electrical flow - as it tries to reach the ground. Because people make excellent conductors, minor electrocution is a common household hazard. Fortunately it is usually more surprising than dangerous and does not require medical attention. However, some basic precautions should be taken to insure that the shock does not interfere with the body's normal electrical impulses including the functions of the brain and the heart. Prolonged exposure to a direct source of electricity can also cause severe burns to the skin and the tissue.
In the event of electrocution do not rush to assist the victim until you are certain that he is no longer in contact with electricity. Otherwise the current will pass through the victim directly to you.
- If at all possible, turn off the source of electricity (i.e. light switch, circuit breaker, etc.) If this is not an option, use non-conductive material such as plastic or dry wood to separate the source of electricity from the victim.
- If the injuries appear serious or extensive, dial 9-1-1.
- Check the victim's vitals signs such as the depth of his breathing and regularity of his heart beat. If either one is effected by exposure to electricity or if the victim is unconscious, begin to perform CPR.
- Treat any areas of the victim's body that may've sustained burns.
- If the victim is responsive and does not appear seriously injured but looks pale or faint, he may be at risk of going into shock. Gently lay him down with his head slightly lower than his chest and his feet elevated.
|
BASIC FIRST AID: HEAD INJURY
Although most minor head injuries caused by a fall or a strike to the head may result in a bruise or a bump and are not dangerous, it is extremely important to pay close attention to the following symptoms:
- Excessive bleeding from an open wound
- Loss of consciousness
- Interruption of breathing
- Prolonged disorientation or apparent memory loss
If you detect any of the above, the victim may have sustained serious head trauma and will require professional medical attention. If that's the case, dial 9-1-1 immediately. Until the ambulance arrives:
- If possible, place the victim in a dim, quite area.
- Lay the victim down with his head and shoulders slightly elevated.
- If the wound is bleeding, dress it with gauze or clean cloth.
- Do not leave the victim unattended.
- If the victim loses consciousness, you may need to perform CPR.
If the injury does not appear serious or extend beyond minor bruising, it should be treated accordingly.
|
BASIC FIRST AID: NOSEBLEED
A human nose is rich with small fragile blood vessels which are susceptible to damage. A nosebleed may be caused by a fall, a strike to the nose, or even from breathing excessively dry air.
If the nosebleed is not a symptom of a more serious injury, it is rarely dangerous and can usually be stopped by applying continuous pressure.
- Do NOT tilt the victim's head backward.
- Have the victim sit or stand upright to slow down the flow of blood.
- Loosen any tight clothing around the victim's neck.
- If possible, have the victim spit out excess saliva - swallowing may disturb the clot and cause nausea.
- Pinch the nostrils shut and press the tip of the nose against the bones of the face.
- Maintain pressure for 5 to 10 minutes.
- Once the bleeding has stopped, the victim should avoid blowing his nose or otherwise straining himself for at least an hour.
|
|
BASIC FIRST AID: PUNCTURE WOUND
Unlike a cut, a puncture wound does not typically result in profuse or excessive bleeding and although painful, may look harmless as the skin around the wound simply closes. But puncture wounds carry a risk of infection and if left unattended can result in serious complications.
Injuries sustained by stepping on a nail that punctures through a shoe are especially prone to infection. If the injury is caused by stepping on a nail or a shard of glass that's been exposed to the elements, it is a good idea to consult a physician who may recommend a tetanus shot or booster.
A bite from a household pet or another person that results in a puncture wound should be considered and treated as serious injury. If the bleeding is heavy or the item that caused the wound appears unsanitary, thoroughly clean the injured area with mild anti-bacterial soap and water and seek professional medical assistance as soon as possible.
If the injury is minor, clean it with soap and water and apply an antibiotic ointment such as Neosporin to prevent infection. Dress the wound with sterile bandage and replace the dressing frequently. It is prudent to keep a close eye on the wound for several days to prevent an onset of an infection from any debris that may've lodged itself deep in the wound. If you notice persistent redness or puffiness or if the wound starts to ooze pus, have the victim consult a doctor right away.
|
A.E.D.
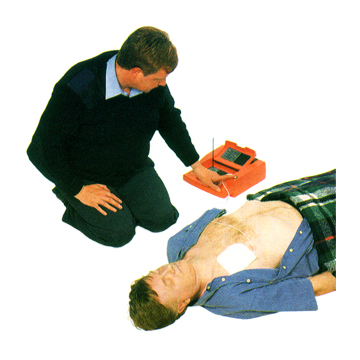
An AED is a small, portable device (figure 1) which uses sophisticated electronics to analyze the victim's heart rhythm, determine whether defibrillation is required, and administer an electric shock to the heart.
Originally designed for use by nonmedical personnel such as officers of the peace, fire fighters, flight attendants, and other lay rescuers with proper training, there is a growing availability of AED's in public places such as schools, airports, libraries, health clubs, and even restaurants and coffee houses.
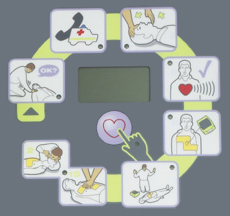
Functionality and features vary slightly from model to model, but most AED's microprocessors are almost fool-proof as they guide the operator through each step with audible and visual prompts (figure 2).
Although research has shown AED's to be approximately 95% accurate - that is the nearly unerring ability to properly assess the need for defibrillation - and most employ multiple safeguards to protect both the victim and the rescuer, fundamental training, including safety and maintenance, is crucial for effective use.
Remember, early CPR is an integral part of providing lifesaving aid to a victim of sudden cardiac arrest. The skills learned in the CPR portion of this course will help to circulate oxygenated blood to the victim's brain until EMS arrives.
How to use AED
- Establish that the victim is experiencing SCA.
- Immediately dial 9-1-1 and provide the operator with all essential information.
- Retrieve AED.
- Attach electrode(s) to the victim as indicated on the diagram.
- Follow prompts and/or directions (figure 3).
|
figure 1
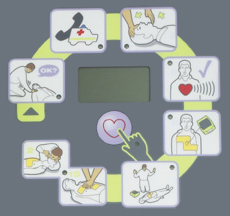
figure 2
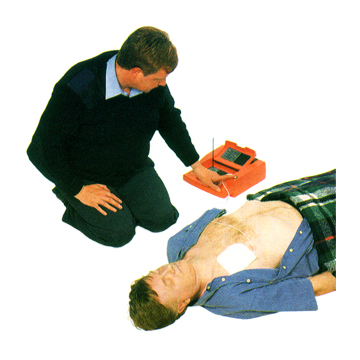
figure 3
|